
Wirbelsäulenerkrankungen: konservative und operative Therapiemöglichkeiten
Stadthalle Landstuhl
WeiterlesenE-Mail senden
Telefon: 06371 84-2701
Wenn die Beschwerden aufgrund der Hüftarthrose durch konservative Maßnahmen nicht mehr zu beherrschen sind und die Lebensqualität deutlich leidet, ist der Zeitpunkt gekommen, an dem eine Gelenkersatzoperation diskutiert werden sollte.
Diese Entscheidung ist immer eine Einzelfallentscheidung, die sich aus der Diskussion zwischen dem behandelnden Arzt und dem Patienten ergibt. Mit dem Einsetzen von künstlichen Hüftgelenken wurde vor etwa 60 Jahren von dem Engländer Sir John Charnley begonnen. Zahlreiche Verbesserungen und die Einführung neuer Materialien haben in den letzten Jahrzehnten dazu geführt, dass die Hüftendoprothetik heute auf einem hohen Niveau steht und die Operation bei den betroffenen Patienten mit großer Zuverlässigkeit zu Schmerzfreiheit und zu verbesserter Funktion führt. Trotzdem ist die Lebensdauer der Endoprothese nicht unbegrenzt sondern je nach verwendetem Material und Aktivitätsniveau mit durchschnittlich 12 – 15 Jahren zu kalkulieren. Unterschiedlichste Einflüsse, die jeder für sich Gegenstand aktueller Forschung sind, wirken auf die Haltbarkeit der Implantate ein.
Ein ganz wesentlicher Gesichtspunkt ist sicherlich die Tatsache, dass die eingesetzten Materialien einem Verschleiß unterliegen und dass dieser umso höher ist, je größer die körperliche Aktivität des betroffenen Patienten ist. So gilt es als gesichert, dass die Endoprothese die längste Haltbarkeit bei weiblichen Patienten jenseits des 70sten Lebensjahres hat und die kürzesten Verläufe männliche, aktive Patienten unterhalb des 60sten Lebensjahres betreffen. Aus dieser Beobachtung ergibt sich die allgemeine Empfehlung, dass die körperliche Belastung und das Aktivitätsniveau eines Endoprothesenträgers auf „normale“ Gehbelastung und „leichte bis mittelschwere“ körperliche Beschäftigung zu reduzieren sind.
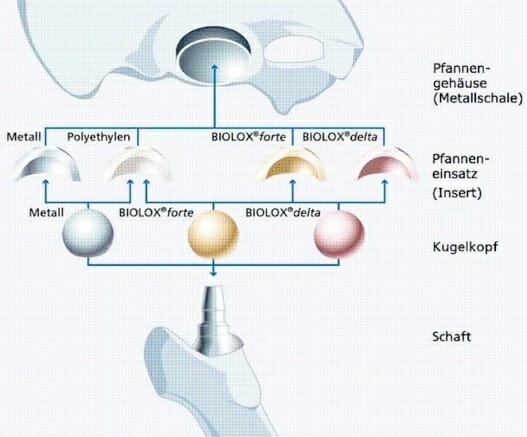
Grundsätzlich kann eine Endoprothese zementfrei oder zementiert eingesetzt werden. Es ist möglich entweder die Pfanne oder den Schaft allein zu zementieren und den anderen Teil der Endoprothese zementfrei zu verankern. In diesem Fall spricht man von einer Hybridversorgung. Für welche Form der Verankerung, für welches Implantat man sich entscheidet ist Gegenstand einer gründlichen Diskussion zwischen Arzt und Patienten. Faktoren, die diese Entscheidung mitbestimmen sind das Alter und das Aktivitätsniveau des Patienten, seine Knochenqualität und die Form seiner Knochen wie auch die zu Grunde liegende Erkrankung, die zur Notwendigkeit des Gelenkersatzes führt (Rheumatische Gelenkentzündung, Arthrose, Hüftkopfnekrose).
Ferner sind Allergien, der allgemeine Gesundheitszustand, größere Unterschiede in der Beinlänge und die in der Klinik verwendeten Endoprothesensysteme in Betracht zu ziehen, wenn diese Entscheidung, die meist sehr individuell ist, getroffen wird.
Neuerdings wird auch dem zunehmenden Wunsch der Patienten nach einer minimal invasiven Operation Rechnung getragen. Hier gilt, dass nicht jeder Schaft für die Implantation über einen solchen schonenden Zugang geeignet ist.
Dieser Begriff ist für die Hüftendoprothetik bislang nicht exakt definiert. Während ein Teil der Fachleute meint, es gehe darum möglichst wenig Knochen zu entfernen, also einen Oberflächenersatz durchzuführen, ist sich die Mehrheit wohl einig darin, dass der Umfang des Muskel- und Weichteilschadens das Kriterium des minimalen Invasivität darstellt. Als unmittelbare Konsequenz lässt sich aus der reduzierten Schädigung der Weichteile eine beschleunigte Rehabilitation ableiten und erwarten. So schön ein kurzer Hautschnitt sein mag, er taugt als Kriterium für die Invasivität einer Operation alleine nicht.
Ein minimal invasiver Hüfteingriff in der Endoprothetik beschreibt also in erster Linie einen Zugang zu dem Gelenk, der zwischen benachbarten Muskeln durchführt und diese dabei nicht beschädigt (sog. Intermuskulärer Zugang). Bei so durchgeführten Operationen lassen sich zusammen mit der Verwendung geeigneter Implantate und Instrumente tatsächlich Hautschnitte von weniger als 10 cm realisieren und überraschend schnelle Verläufe in der Rehabilitation sind die Regel. Diese Form der Hüftchirurgie ist nicht für alle Patienten gleichermaßen geeignet.
Das oberste Ziel eines Hüftgelenkersatzes bleibt immer ein Implantat so gut zu verankern und so korrekt einzusetzen, dass es die größtmögliche Lebensdauer hat. Unter keinen Umständen darf also der minimal-invasive Zugang dazu führen, dass hier falsche Kompromisse gemacht werden und dadurch die eigentlichen Ziele des Gelenkersatzes gefährdet werden.
Wir verwenden minimal-invasive Hüftzugänge seit 2007 mit immer zunehmender Häufigkeit bei Patienten mit geeignetem Körperbau und mit geeigneter Knochenform. Bei schwierigen anatomischen Verhältnissen oder bei besonderen knöchernen Voraussetzungen ist ein konventioneller Hüftzugang – gerade im Hinblick auf die Haltbarkeit der eingesetzten Prothese – die bessere Alternative.
Alle sogenannten konventionellen Hüftzugänge werden bei uns durchgeführt. Die Entscheidung ob ein seitlicher oder ein hinterer Zugang zur Anwendung kommen ist wiederum individuell und hängt davon ab, welche anatomischen Gegebenheiten vorliegen und welches Implantat zur Anwendung kommen soll.
In der Knieendoprothetik ist die Verwendung der Navigation bei uns seit 2007 Standard. Auf Grund der guten Erfahrungen, die wir machen konnten, haben wir auch in der Hüftendoprothetik mit der Verwendung der Navigation begonnen. Die bisherigen Ergebnisse sind sehr vielversprechend und wir sehen derzeit die folgenden Vorteile der Hüftnavigation im Vergleich zu der konventionell eingesetzten Hüfte:
Seit 2007 arbeiten wir in der Endoprothetik hauptsächlich mit der Fa. Amplitude zusammen. Fast alle Knieendoprothesen und drei Viertel der Hüftendoprothesen, die wir einsetzen stammen von diesem Hersteller. Mehr als 90% der Implantationen werden ohne Knochenzement, das heißt zementfrei durchgeführt.
Für besondere Situationen, beispielsweise bei weichem, osteoporotischem Knochen, kann das Einzementieren eines oder beider Implantate erforderlich werden.
Dr. Werner Hauck: Ich arbeite seit 1984 als Arzt und bin mit Gelenkoperationen von Anfang an vertraut. Die AMIS Methode wende ich seit über 8 Jahren an und habe bisher ca. 1.000 Hüften nach dieser Methode ersetzt. Insgesamt habe ich mehr als 4.000 Gelenkoperationen an Hüft- und Kniegelenk durchgeführt.
Dr. Werner Hauck: Järhlich werden ca. 350 neue Hüftgelenke eingesetzt.
Dr. Werner Hauck: Es werden etwa 1/3 nach der AMIS Methode durchgeführt.
Dr. Werner Hauck: Die Entscheidung welches Implantat und welcher Zugang zur Hüfte verwendet wird, ist von mehreren Faktoren abhängig: In erster Linie sind die anatomischen Voraussetzungen des Patienten zu betrachten, der BMI sollte nicht über 30 sein und im Bereich des geplanten Hautschnittes, also in der Leistenregion, dürfen keine Hautirritationen vorhanden sein. In zweiter Linie spielen die Form und die Stabilität der Knochen eine Rolle. Das Alter und Begleiterkrankungen sind nicht wirklich von Bedeutung.
Dr. Werner Hauck: Üblicherweise werden beim Einsetzen eines neuen Hüftgelenks einzelne Muskeln und auch dazugehörige Nerven durchtrennt bzw. beschädigt. Die AMIS Methode stellt eine überzeugende Entwicklung in der Hüft-Endoprothetik dar. AMIS > Anterior Minimal Invasive Surgery. Der AMIS Zugang ist der einzige Weg zum Hüftgelenk, bei dem weder Muskulatur durchtrennt noch Nerven beschädigt werden. Er führt schräg vorne, seitlich der Leistenbeuge zwischen dem Versorgungsgebiet der beiden Hauptnerven des Oberschenkels in das Gelenk und vermeidet dadurch jede Beeinträchtigung. Die AMIS Methode ist eine sehr schonende Behandlungsmethode bei der der Patient weniger Schmerzen hat und die Erholung deutlich schneller einsetzt.
Dr. Werner Hauck: Die Vorteile liegen in einer kurzen Verweildauer im Krankenhaus und einer schnellen Rehabilitation, das heißt man bleibt ca. 5-7 Tage im Krankenhaus und kehrt nach weiteren 3 Wochen mit Rehabilitation bzw. Physiotherapie wieder in sein normale Leben zurück. Viele unserer Patienten beginnen in der zweiten Woche nach der OP im angegliederten Zentrum für Rehabilitation (ZAR) mit ihrer Reha.
Dr. Werner Hauck: Fast alle Patienten benötigen die Krücken meist nur 3 Wochen. In Einzelfällen ist es sinnvoll diese für ein besseres/harmonischeres Gangbild länger zu nutzen. Immer wieder erwischen wir Patienten schon in den ersten Tage ohne Krücken, weil sie sich einfach gut und schmerzfrei fühlen. Aber das wollen wir nicht wirklich.
Dr. Werner Hauck: Es ist möglich wieder Sport zu machen gibt aber zu empfehlende Sportarten und Sportarten, die nach so einer OP nur bedingt zu empfehlen sind.
Dr. Werner Hauck: Zu empfehlen sind Sportarten wie z. B. Golf, Wandern, Schwimmen, Tanzen etc. Der ideale Sport ist Nordic Walking. Nicht zu empfehlen sind Stop&Go Sportarten wie Tennis und Joggen. Allerdings kommt es hier auf die Intensität, mit der man die Aktivitäten betreibt an. Das sollte dann von Fall zu Fall individuell besprochen werden.
Dr. Werner Hauck: Die meisten Eingriffe werden mit einer Allgemeinanästhesie durchgeführt aber es ist auch möglich die OP in Spinalanästhesie durchzuführen.
Dr. Werner Hauck: Mein Team besteht aus 11 Ärzten, 14 Physiotherapeuten und 40 Krankenschwestern und Pflegern. Seit 2001 bin ich Chefarzt der orthopädischen Abteilung und Leiter der Abteilung für Physikalische Therapie.
Dr. Werner Hauck: Jährlich behandeln wir im Fachbereich der Orthopädie 2.500 stationäre Patienten, ungefähr 5.000 ambulante Patienten und natürlich zahlreiche Notfälle.
Dr. Werner Hauck: Das Krankenhaus hält alle modernen Diagnoseverfahren vor, insbesondere in der Radiologie mit 24 Stunden Verfügbarkeit von MRT, CT und Angiographie. Für Patienten mit kritischen Gesundheitsverhältnissen haben wir eine Intensivstation mit entsprechenden Fachärzten und einer „State of the Art“ Ausstattung. Spezialisten aus anderen Fachdisziplinen stehen ebenfalls zur Verfügung. Die Patienten sind im Einbettzimmer untergebracht und haben TV, W-LAN und Telefon. Die meisten unserer Mitarbeiter sprechen gut Englisch.
Ergänzend zu unseren Präsenzveranstaltungen finden Sie die Vorträge von Dr. Sascha Schläger als Videos in unserer Mediathek, sodass Sie sich zu den Themen Arthrose, Knie- und Hüftgelenksersatz, Osteoporose sowie Wirbelsäulenerkrankungen informieren können: Zur Mediathek wechseln